Spondylolysis
Spondylolysis
Overview | Causes | Symptoms | Diagnosis | Treatment | FAQ
Overview
Spondylolysis relates to instability of specific bones in the low back. It a very common cause of back pain, particularly in adolescents. Gymnasts who perform routines that bend and arch the back are often victims of spondylolysis or spondylolisthesis.
[top]
Causes
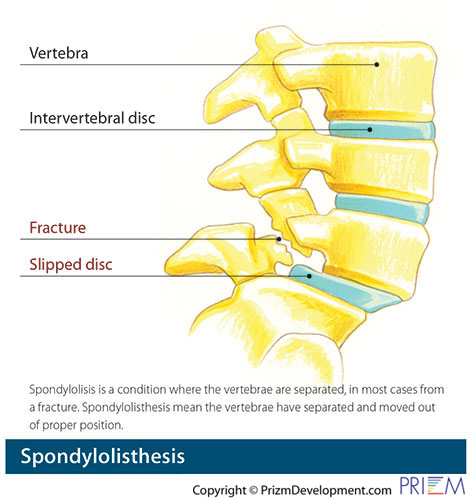
Spondylolisthesis and spondylolysis are caused by joint instability in the low back. The rear part of spinal vertebrae has facet joints that act as hinges, allowing our spines to twist and bend. Sometimes, however, the posterior element can crack. Either from heredity or wear and tear, part of the posterior element called the pars interarticularis can crack, causing the vertebrae to slip forward out of its correct position. Spondylolysis occurs when the PARS hinge is cracked, but the vertebrae is still in its correct position. Spondylolisthesis occurs when the cracked PARS has allowed the vertebrae to slide forward out of its correct position. If left untreated, spondylolysis can lead to spondylolisthesis.
[top]
Symptoms
Interestingly, in many cases, spondylolisthesis may have no symptoms, so most people may not know they have it. Back pain is the most common symptom, particularly in the lower back. This back pain may be mistaken for a muscle strain. Muscle spasms that occur as a result of spondylolysis may cause an overall feeling of stiffness in the back and may effect posture.
[top]
Diagnosis
Outlined below are some of the diagnostic tools that your physician may use to gain insight into your condition and determine the best treatment plan for your condition.
- Medical history: Conducting a detailed medical history helps the doctor better understand the possible causes of your back and neck pain which can help outline the most appropriate treatment.
- Physical exam: During the physical exam, your physician will try to pinpoint the source of pain. Simple tests for flexibility and muscle strength may also be conducted.
- X-rays are usually the first step in diagnostic testing methods. X-rays show bones and the space between bones. They are of limited value, however, since they do not show muscles and ligaments.
- MRI (magnetic resonance imaging) uses a magnetic field and radio waves to generate highly detailed pictures of the inside of your body. Since X-rays only show bones, MRIs are needed to visualize soft tissues like discs in the spine. This type of imaging is very safe and usually pain-free.
- CT scan/myelogram: A CT scan is similar to an MRI in that it provides diagnostic information about the internal structures of the spine. A myelogram is used to diagnose a bulging disc, tumor, or changes in the bones surrounding the spinal cord or nerves. A local anesthetic is injected into the low back to numb the area. A lumbar puncture (spinal tap) is then performed. A dye is injected into the spinal canal to reveal where problems lie.
- Electrodiagnostics: Electrical testing of the nerves and spinal cord may be performed as part of a diagnostic workup. These tests, called electromyography (EMG) or somato sensory evoked potentials (SSEP), assist your doctor in understanding how your nerves or spinal cord are affected by your condition.
- Bone scan: Bone imaging is used to detect infection, malignancy, fractures and arthritis in any part of the skeleton. Bone scans are also used for finding lesions for biopsy or excision.
- Discography is used to determine the internal structure of a disc. It is performed by using a local anesthetic and injecting a dye into the disc under X-ray guidance. An X-ray and CT scan are performed to view the disc composition to determine if its structure is normal or abnormal. In addition to the disc appearance, your doctor will note any pain associated with this injection. The benefit of a discogram is that it enables the physician to confirm the disc level that is causing your pain. This ensures that surgery will be more successful and reduces the risk of operating on the wrong disc.
- Injections: Pain-relieving injections can relieve back pain and give the physician important information about your problem, as well as provide a bridge therapy.
[top]
Treatment
Conservative treatments should always be considered first when treating spondylolysis. Nonsurgical treatment methods include resting and refraining from usual activities, taking anti-inflammatory medication, and incorporating a stretching and strengthening program. While ligaments and muscles can help hold the vertebrae in place, over time, surgery may be necessary to install surgical instrumentation or bone grafts that lock the vertebra in place so that it does not slide out of position and damage the spinal nerves. Surgery may involve a fusion and/or screws and rods.
[top]
FAQs
How do I know if I am at risk for spondylolysis?
Those with a family history of spondylolysis or weak vertebrae are more susceptible to developing the condition. Also, athletes involved in activities that place a great deal of stress on the back, such as football players and weight lifters, are at greater risk for fracturing the vertebrae, encouraging slippage.
[top]